Exploring the Depths of Epidermolysis Bullosa: Understanding a Rare Genetic Skin Disorder
- Joseph Powl

- Jul 10, 2024
- 4 min read
In the realm of dermatology, few conditions are as devastating and complex as epidermolysis bullosa (EB). This group of genetic disorders, often described as “butterfly skin” due to the fragile nature of the skin, presents a profound challenge to those affected and their families. Epidermolysis bullosa encompasses a range of subtypes, each with its own set of symptoms and severity, but all share the common feature of extreme skin fragility.
What is Epidermolysis Bullosa?
Epidermolysis bullosa is a group of inherited disorders characterized by extremely fragile skin that blisters and tears easily. The condition arises from genetic mutations that affect the proteins responsible for holding the skin layers together.
There are several forms of EB, including:

Epidermolysis Bullosa Simplex (EBS): This form primarily affects the outer layer of the skin (epidermis) and is usually less severe.
Dystrophic Epidermolysis Bullosa (DEB): In this form, the separation occurs in the deeper layers of the skin, leading to more severe symptoms.
Junctional Epidermolysis Bullosa (JEB): This form affects the layer where the epidermis and dermis meet and is often more severe.
Kindler Syndrome: A rarer form of EB that combines features of other types and involves photosensitivity and skin fragility.
The Appearance and Symptoms:
The hallmark of epidermolysis bullosa is the formation of blisters and sores on the skin and mucous membranes. These blisters can develop spontaneously or with minimal trauma. The severity of symptoms varies widely among the different forms of EB:
Blistering: Blisters can appear on any part of the body, including internal mucous membranes. They can cause significant discomfort and pain.
Skin Erosion: Repeated blistering can lead to skin erosion, infection, and scarring.
Nail and Hair Abnormalities: Some forms of EB can affect the nails and hair, leading to deformities and loss of function.
Systemic Complications: Severe cases of EB can involve other organs, leading to complications such as esophageal strictures or respiratory issues.
Statistics and Prevalence:
Epidermolysis bullosa is a rare condition with an estimated prevalence of 1 in 50,000 live births worldwide (Fine, J.D., 2016). The prevalence of specific types of EB varies:
Epidermolysis Bullosa Simplex (EBS): Estimated to occur in 1 in 100,000 births (Uitto, J., 2011).
Dystrophic Epidermolysis Bullosa (DEB): Estimated at 1 in 500,000 births (Fine, J.D., 2016).
Junctional Epidermolysis Bullosa (JEB): Approximately 1 in 200,000 births (Kern, J.S., 2015).
Kindler Syndrome: Very rare, with fewer than 50 cases reported worldwide (Junker, J.P., 2014).
Diagnosis and Management:
Diagnosis of epidermolysis bullosa typically involves a combination of clinical evaluation and genetic testing. A skin biopsy can be performed to examine the structure and location of the blistering.
Management of EB is primarily supportive and aims to minimize blistering, prevent infections, and manage pain:
Wound Care: Proper wound care is critical to prevent infection and promote healing. This includes the use of gentle, non-adherent dressings and topical antibiotics.
Pain Management: Pain associated with blistering and skin damage is managed with analgesics and other pain relief strategies.
Nutritional Support: Individuals with severe EB may have difficulty eating due to mouth and esophageal blistering, requiring nutritional support and dietary adjustments.
Preventive Measures: Reducing friction and trauma to the skin through careful handling and protective clothing is essential.
Advances in Treatment and Research:
Research into epidermolysis bullosa is ongoing, with several promising developments:
Gene Therapy: Scientists are exploring gene therapy techniques to correct the underlying genetic mutations that cause EB. Early clinical trials have shown some promise in treating certain forms of the disorder (Titeux, M., et al., 2014).
Wound Healing Technologies: Advances in wound care technologies, including bioengineered skin grafts and novel dressings, are improving the management of EB wounds (Grootenboer-Mignot, S., et al., 2015).
Supportive Therapies: New approaches in pain management, nutritional support, and psychosocial care are enhancing the quality of life for individuals with EB (Kern, J.S., 2015).
Living with Epidermolysis Bullosa:
Living with epidermolysis bullosa presents significant challenges, but with advances in medical care and support, individuals with EB can lead fulfilling lives. Comprehensive care teams, including dermatologists, wound care specialists, nutritionists, and psychologists, play a crucial role in managing the condition and improving the quality of life.
Conclusion:
Epidermolysis bullosa is a rare and complex skin disorder with a profound impact on those affected. Understanding the condition and the ongoing advancements in treatment and research offer hope for better management and improved outcomes. As the field of dermatology continues to evolve, so too does the potential for new therapies that can transform the lives of individuals living with EB.
Citations:
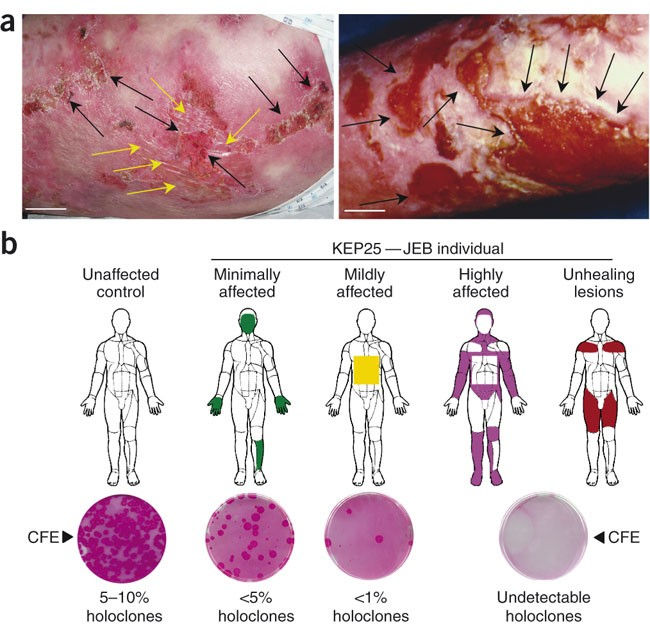
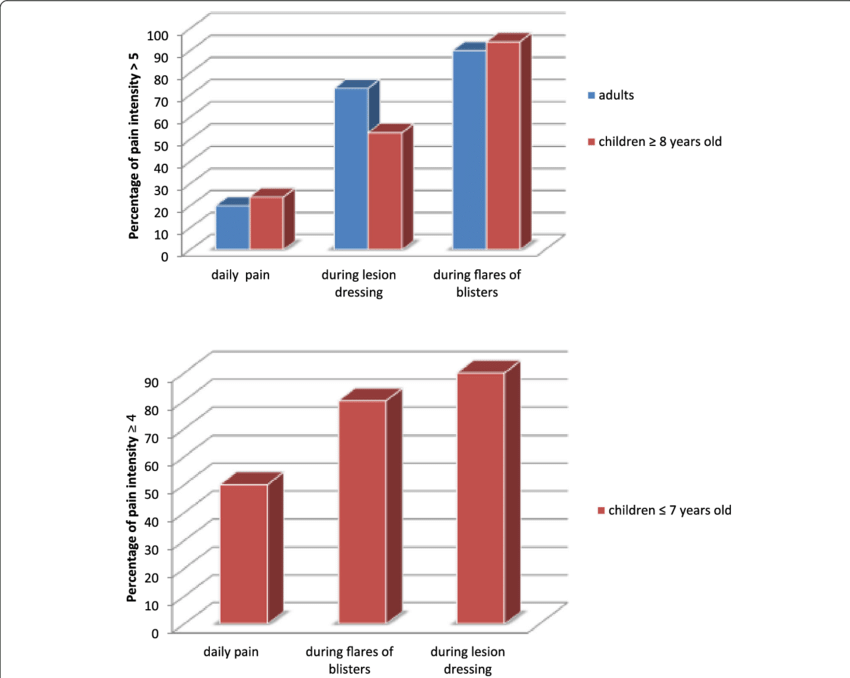
Images:
Patient with Epidermolysis Bullosa: Photo Credit due to Mayo Clinic, asked for permission to use photo, no changes were made to the image.
Assessment of the level of EB: Photo Credit due to ResearchGate, asked for permission to use photo, no changes were made to the image.
Sources:
Fine, J.D. (2016). Epidermolysis Bullosa. GeneReviews. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK1243/
Uitto, J. (2011). Epidermolysis Bullosa Simplex: Pathogenesis and Clinical Features. Journal of Investigative Dermatology, 131(6), 1466-1473.
Kern, J.S. (2015). The Clinical Spectrum of Junctional Epidermolysis Bullosa. Dermatologic Clinics, 33(3), 407-416.
Junker, J.P. (2014). Kindler Syndrome: A Rare Epidermolysis Bullosa Variant. Dermatology Online Journal, 20(8).
Titeux, M., et al. (2014). Gene Therapy for Epidermolysis Bullosa. Molecular Therapy, 22(1), 22-34.
Grootenboer-Mignot, S., et al. (2015). Advances in Wound Care Technologies for Epidermolysis Bullosa. Wound Repair and Regeneration, 23(5), 728-735.
743 views



Comments